What is a Bone Graft?
Dental implants are designed to replace lost teeth and improve jaw function. However, if a tooth has been absent for an extended period, the jawbone might start to weaken. Insufficient bone density can lead to the failure or loosening of dental implants. Bone grafting, a simple surgical technique, replenishes bone tissue, enabling the jawbone to adequately support the dental implant.
“Is a Bone Graft Right for Me?”
If you’re considering a dental implant, the first step is to visit our Sarasota dental implant clinic for an initial consultation. In this exam, our expert will assess your oral health and perform an x-ray of your jawbone to check if it has adequate density to hold the implant. Should your jawbone seem insufficient for the implant, a bone graft might be suggested as a solution.
Various types of bone grafting materials are available, all of which are clinically verified and safe for encouraging bone tissue regeneration. These materials serve as a framework that facilitates the growth of your natural bone tissue, ultimately taking the place of the graft material entirely.
Autograft
One widely used bone grafting method is the autograft. In this procedure, bone material is sourced from your own body. Distinct from other graft types, autografts require two surgical areas: one for harvesting the bone material and another where it is transplanted.
Allograft
An allograft involves using donor bone tissue obtained from a tissue bank. This tissue, sourced from a deceased donor, is processed and prepared in a laboratory.
Xenograft
This type of graft is akin to an allograft, but it utilizes bone tissue sourced from an animal.
Alloplast
The Bone Grafting Process
Consultation
Before proceeding with your dental bone graft, your doctor will first assess your suitability for the procedure. At your initial consultation, they will evaluate the health of your teeth and gums and perform an x-ray of your jawbone. If it’s determined that a bone graft could be beneficial for your bone structure, we will then arrange a date for your surgery.
Procedure
Initially, your doctor will administer a local anesthetic to numb the region of your mouth where the graft will be placed, ensuring you feel no discomfort during the procedure. After numbing the area, a small cut is made in the gums to expose the jawbone. The doctor will then clean and sterilize this area before applying the bone grafting material. Finally, the gum tissue is repositioned over the graft site and securely sutured.
Aftercare
Although the surgical procedure typically involves minimal pain, you might feel some swelling or discomfort once the anesthetic diminishes. These symptoms are normal and should subside within a few days. To help manage any pain, your doctor may prescribe pain medication or antibiotics. It’s also common to notice small fragments of bone material at the incision site in the following days; this is a normal part of the healing process and not a cause for concern. For any questions or concerns, feel free to reach out to our office.
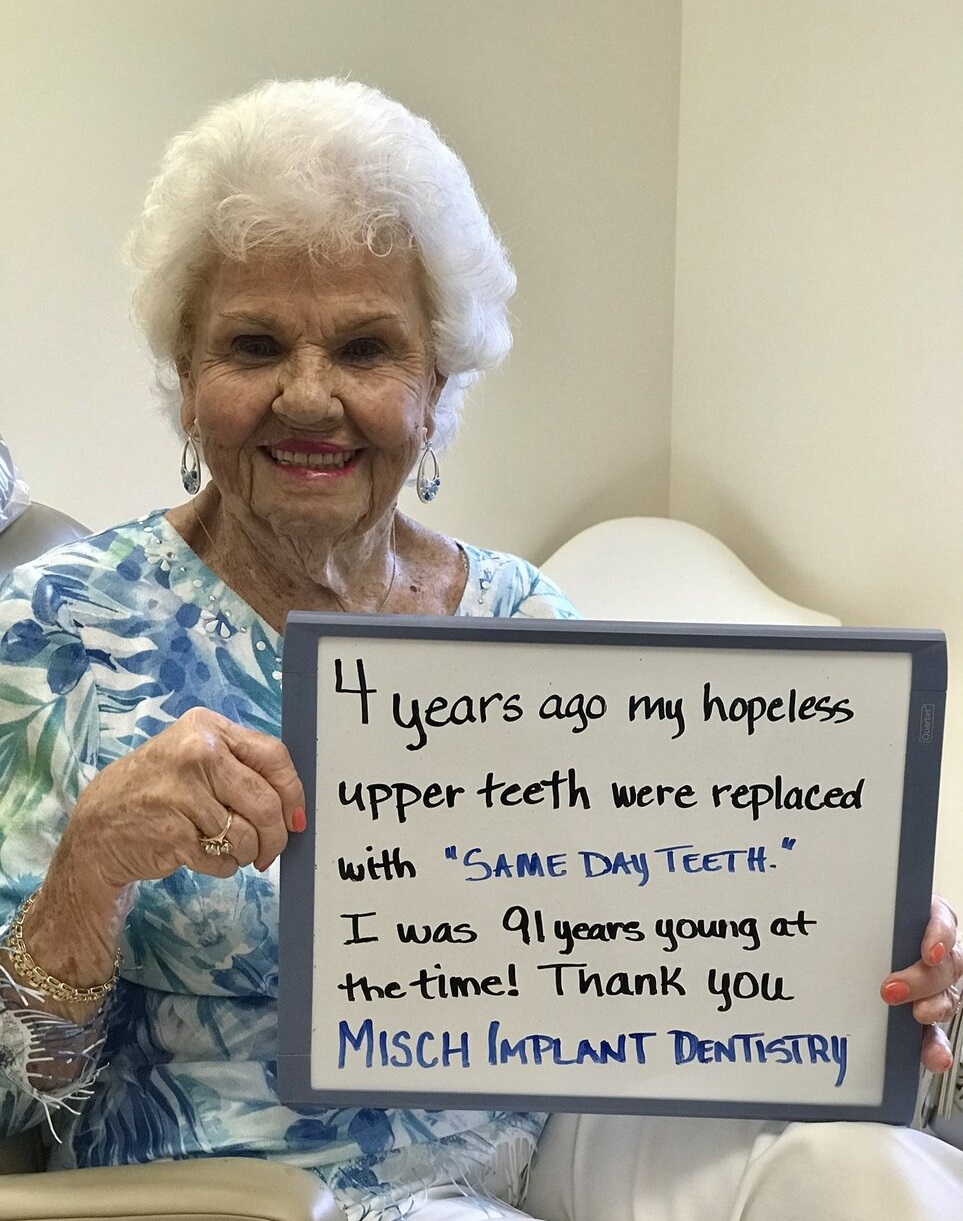
Contact us today
to schedule an initial consultation & exam.
Your consultation will include an examination of everything from your teeth, gums and soft tissues to the shape and condition of your bite. Generally, we want to see how your whole mouth looks and functions. Before we plan your treatment we want to know everything about the health and aesthetic of your smile, and, most importantly, what you want to achieve so we can help you get there.
Frequently Asked Questions
Dental bone grafts boast a high rate of success, but failure is always a possibility. Contact your doctor if you notice any of the following symptoms:
- Discomfort worsens after the first week
- Discharge from the operation site
- Gum recession
While the surgical site shouldn’t take more than a week or two to heal, it may take anywhere from three to nine months before the bone graft has established sufficient bone mass. Your age, dental health, and the type of graft are all factors that can affect the recovery time.
In your bone grafting procedure, the doctor will use a local anesthetic to fully numb the area, ensuring you feel little to no discomfort during the surgery. After the procedure, as the anesthetic wears off, you might experience some minor pain and swelling. To help manage this, your doctor may prescribe pain medication. Typically, discomfort should significantly reduce or disappear within a week. If you notice an increase in pain or swelling after a week, it’s important to get in touch with your doctor.
Bone grafts usually don’t necessitate sedation, as local anesthesia is generally sufficient to prevent discomfort. However, for patients experiencing significant dental anxiety, sedation may be considered. Common sedation methods include nitrous oxide (laughing gas), oral sedation, and IV sedation. It’s important to discuss these options with your doctor to determine if sedation is appropriate for your situation.